Covid-19: loss of smell and taste
The loss of the sense of smell and taste is one of the most common side effects of a Covid infection - and a disaster, especially for chefs and sommeliers. But why does this disorder develop?
»From one day to the next, I could no longer smell or taste anything,« says Benjamin Edthofer, who caught an omicron infection at the end of January. Especially bad in his case: Edthofer is a sommelier at the wine bar Heunisch und Erben in Vienna’s third district. »I didn't actually have any symptoms. I wasn't sick,« Edthofer recalls, »but I suddenly couldn't distinguish four completely different wines by smell. All four smelled completely the same to me, or rather, they smelled like nothing at all.«
Total loss of smell
What is bad for anyone turns out to be a disaster for someone who has to have a functioning olfactory system for professional reasons. Edthofer: »In the beginning, I only perceived odours five percent of the time. I could hang up my job with that. Fortunately, it got better from week to week. I estimate that my sense of smell has now returned to 60 percent. But I still can´t smell as well as I could before.«
In such a case, doctors speak of anosmia. A distinction is made between functional and complete anosmia. In functional anosmia, the sense of smell is so severely impaired that it can no longer be used meaningfully in everyday life, even if a few odours can still be perceived occasionally, faintly or briefly. However, this residual ability to smell is insignificant. In the case of complete anosmia, the sense of smell is completely disabled, which means that there is no residual ability to smell.
Whether functional or complete anosmia, the everyday experience of those affected is simply: »I can no longer smell.« So no more asking your nose whether the milk is sour, the T-shirt from the day before is smelly or the perfume gift from your partner is good or disgusting. In addition, many people with anosmia have problems with their sense of taste: most of them can taste salty, sour, sweet and bitter things normally, but can no longer distinguish between certain flavours. This requires not only the taste receptors but also the olfactory receptors on the tongue; only when they work together can a flavour fully unfold.
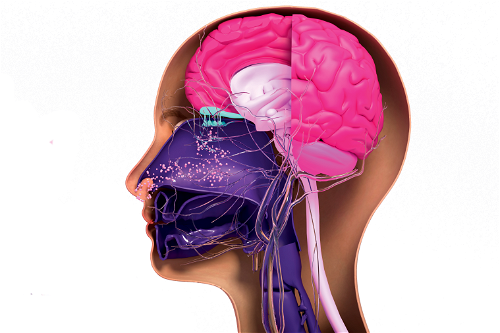
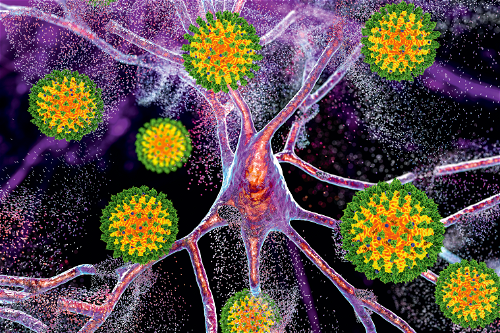
But how do such disturbances in the sense of smell occur? Two types of receptors play an important role: the ACE2 receptors (angiotensin-converting enzyme 2) and the neurolipin-1 receptor serve the Covid viruses as an entry port into the sensitive cells.
A particularly high density of neurolipin-1 receptors is found in the human nose in the olfactory epithelium. Researchers have now discovered that coronaviruses can even penetrate the brain. In this way, virus particles could reach the central nervous system since there is a direct connection to the brain via the olfactory epithelium. Whether the viruses take this direct route via the olfactory epithelium and to what extent this transport route is suppressed by the immune system in most people has not yet been proven.
By the way, smell and taste disorders can also occur during influenza, but the mechanisms are different. In the case of influenza or flu-like infection, the patients have a cold, their nose is swollen shut and when the fever is gone, some lose their sense of smell for a short time, which then quickly returns. Covid patients are different: they can usually breathe very well through their nose but cannot smell from the beginning of the infection.
Interestingly, the olfactory system is also the only sensory system where the sensory cells are neurons, while the gustatory system is made up of skin cells, mainly on the tongue. It seems that the neurons in the olfactory system die off during a Covid infection. Fortunately, the neurons in the olfactory system can renew themselves, but this can take several months.
What therapies are available?
And what can be done about long-term smell and taste disorders? Researchers at the University of East Anglia in the UK looked into this in a recent study and concluded: Not only medication but above all intensive olfactory training helps Long Covid patients, which is why more and more experts recommend structured olfactory training for post-infectious olfactory disorders. The exact structure of the training can vary and is discussed with the patient in each case. For example, the patient can sniff twice a day for several weeks at olfactory training sticks that contain a certain scent (e.g., lemon, clove, eucalyptus).
This training of the sense of smell can be supported by associating each smell with pictures or words. When sniffing the lemon pen, for example, patients can look at the picture of a lemon and say the word lemon in their mind or out loud. In this way, the olfactory impression is better remembered. However, it is still unclear whether the sense of smell recovers 100 percent in all patients.
Especially in short pieces, watch out for the tendency to repeat vocabulary items, especially ones that are not needed at all. In this case, the word 'so-called' is not needed. Although one of its meanings is 'commonly named', it is not needed when we are simply stating the name of something, particularly its scientific name. Further, the word also means 'falsely or improperly named', and this negative connotation can come to people's minds when the word is used where it is not needed.
Hintergrund: So riechen und schmecken wir
»Das kann auch sehr lange dauern«
Der Wiener Universitätsprofessor Felix Stockenhuber, Facharzt für Innere Medizin, über Geruchs- und Geschmacksstörungen bei einer Corona-Infektion.

Falstaff: Geruchs- und Geschmacksverlust ist ein gefürchtetes Phänomen
bei einer Corona-Erkrankung. Aber ist die Gefahr bei der Omikron-Variante genauso groß wie bei Delta?
Felix Stockenhuber: Man hat den Eindruck, dass diese Störung bei Omikron etwas weniger häufig ist. Aber auch bei Omikron tritt die Störung über ACE2-Rezeptoren in der Riechschleimhaut ein. Dort nutzen die Spike-Proteine der Corona-Viren diese Andockstellen als Eingangspforte, um in die Zellen einzudringen und sich zu vermehren.
Wo genau spielt sich das ab?
Im oberen Nasenbereich, da ist eine Stelle, das sogenannte Riechepithel, wo sich die ACE2-Rezeptoren befinden. Es gibt ja auch bei einer Grippe diese Störung, allerdings ist es bei der Grippe so, dass es zu einer Geruchsstörung kommt, weil die Nase zugeschwollen ist und man nicht durchatmen kann. Man bemerkt die Störung damit gar nicht. Bei Covid bleibt die Nase aber oft frei, die Geruchs- und Geschmacksstörung gehört deshalb zu den ersten, manchmal ist sie auch das ausschließliche Symptom. Das ist dann meist nach ein, zwei Wochen wieder vorbei.
Aber gibt es nicht auch Fälle, wo das länger gedauert hat …
Ja, das stimmt. Man weiß auch mittlerweile, wovon das abhängt. Man hat nachweisen können, dass in manchen Fällen immer noch genetische Substanzen des Virus in der Nase sind. Auch über einen längeren Zeitraum. Die Betroffenen haben an dieser Stelle im Nasenbereich immer noch Viren, sie können möglicherweise immer noch infektiös sein. Man weiß auch, dass Raucher häufiger betroffen sind als Nichtraucher.
Wird man in solchen Fällen noch positiv getestet?
Wahrscheinlich nicht, es sind ja nur noch wenige Viren vorhanden, die bei einem PCR-Test meist nicht mehr erkannt werden. Das führt dann zu einem negativen Ergebnis. Das Virus ist ja heimtückisch. Es gibt mittlerweile auch Studien, aus denen hervorgeht, dass das Virus von einer Gehirnzelle zu einer anderen wandert (vom Riechepithel gibt es eine direkte Verbindung zum Gehirn, Anm.). Das Immunsystem hat da oft gar keine Chance hinzukommen.
Wie lange kann eine Geruchs- und Geschmacksstörung schlimmstenfalls dauern?
Man weiß inzwischen, dass in fünf bis zehn Prozent der Fälle die Störung sehr lange dauert. Es wird angenommen, dass es sich dabei eben um Viren handelt, die noch vorhanden sind. Es ist nur eine kleine Menge an Viren, aber sie sind eben länger vorhanden. Es gibt Fälle, bei denen die Störung ein Jahr und noch länger gedauert hat. Der Geruchssinn kommt dann erst wieder langsam zurück, es handelt sich da um eine Anosmie durch Covid. Bei einer Anosmie hat man auch eine Art Missempfinden des Geruchs, eigentlich positiv empfundene Gerüche werden dann als negativ und ekelhaft empfunden. Manches riecht dann plötzlich etwa wie eine Kloake – das sind Phantomgerüche, die erst langsam wieder verschwinden, manchmal aber auch gar nicht mehr. Mann muss aber auch sagen, dass ältere Menschen ohnehin schon einen reduzierten Geruchssinn haben.
Für einen Koch oder einen Sommelier ist das jedenfalls besonders unangenehm …
Ja, mit Sicherheit. Ich habe einen Patienten, der produziert Salzgebäck. Der kann das jetzt nicht mehr abschmecken. Der riecht und schmeckt das Salzgebäck einfach nicht mehr.
Gibt es entsprechende Therapien?
Ja, es gibt die Möglichkeit, dass man örtlich Vitamin A einsetzt in Form von Nasentropfen, und auch Vitamin D. Da ist aber die Datenlage noch schwach. Es gibt auch Geruchstraining. Dabei werden in der Früh und am Abend jeweils eine Minute lang bestimmte Gerüche trainiert. Ich habe auch ein Sauerstoffzelt für meine Patienten. Diese hyperbare Sauerstofftherapie hilft normalerweise bei der Wundheilung, bei Knochenödemen und Tauchunfällen. Und es gibt auch positive Erfahrungen bei Long Covid damit.